Debunking Pro-Vaccine Arguments in the Kirsch/Wilf $2M Debate
The following is a detailed rebuttal of the arguments presented by Wilf for the pro-vaccine side in this high-stakes discussion.
Steve Kirsch and Wilf are engaged in a multi-round debate with $2 million at stake. The central question: Do the “COVID-19 vaccines” provide a net benefit? Based on the evidence I have reviewed, my position is clear: The covid-19 vaccines have not been shown to have a net benefit. In fact, the data suggests a relatively weak but discernible net harm. This analysis focuses solely on identifying flaws in Wilf’s pro-vaccine position.
General Remarks & Fallacies by Wilf
Wilf begins his essay by asserting that “vaccines work,” drawing a comparison to similar products from the past. However, this argument relies on a logical fallacy: it assumes that the assumed effectiveness (and mechanism) of other vaccines inherently proves the effectiveness of the current ones. This raises a critical question: what if past vaccines also didn’t work as claimed? Furthermore, Wilf argues that the majority of people believing in vaccines makes it unlikely for them to be wrong. Yet, this is another fallacy—an appeal to popularity—offered without supporting evidence.
Later, Wilf remarks that in the past, death signals from vaccination would have been detected. However, concluding that the same would inevitably occur this time is a flawed assumption and represents a logical fallacy.
In addition, he highlights that the mechanism of action causing harm or death would not be unknown. Contrarily, Pfizer explicitly states that ‘the exact immunologic mechanism that confers protection against SARS-CoV-2 is unknown.’ This implies they do not fully understand how their product is even supposed to work.
In contrast, there are at least two plausible mechanisms for harm:
Direct cell inflammation and potential cell death caused by lipid nanoparticles (LNP), as described by Ndeupen et al., 2021.
The immune system attacks cells that produce the “supposedly foreign” or harmful antigen. This occurs due to the widespread distribution of lipid nanoparticles (LNPs) throughout the body, leading to the destruction of cells in multiple organs, including the heart and brain.
Moreover, vaccine-critical studies have been subjected to significantly more scrutiny, suppression, and even outright banning by journals and certain authors. This double standard raises valid concerns about bias in the academic and scientific discourse surrounding vaccines.
Wilf also overlooks two critical motivations that shape the broader vaccine narrative:
Government Objectives: Governments primarily aim to calm the public and maintain order during crises. Tools like masks, tests, and vaccines serve as tangible measures to reassure the public. However, whether these tools are effective is often a secondary concern, as the primary motivation of governments is typically to control the narrative and preserve authority.
Pharmaceutical Industry Incentives: The incentives for pharmaceutical companies are clear. With liability protections in place, these companies effectively operate with a blank check, profiting immensely as long as public fear—and thus demand—can be sustained. This is facilitated by significant influence over the media, where the pharmaceutical industry is the major force in advertising spending. Compounding this issue, these companies often conduct their own trials, creating an inherent conflict of interest that undermines trust in the results.
These considerations highlight critical gaps in Wilf’s arguments and underscore the importance of scrutinizing both the evidence and the motivations driving the vaccine narrative.
Establishing the Meaning of Net Benefit
Before addressing and debunking each of the points raised by Wilf, it’s important to first revisit the objectives of this debate and clarify what constitutes valid proof in this context. The legal framework how cause can only be established by prospective double-blinded, placebo RCT’s - and not by con-founded observational studies - was recently laid out by vaccine attorney Aaron Siri on Tucker Carlson’s podcast.
The term Net Benefit implies that the benefits must significantly outweigh the harms, meaning notably more lives are saved than harmed.
There are three main types of evidence to consider to answer the question of net-benefit:
1. Studies that prove causality: These include prospective, double-blind, placebo-controlled trials, which are the gold standard for establishing cause and effect.
2. Confirmed reports and harm statistics: Documented cases and data that provide evidence of adverse outcomes.
3. Post-marketing studies: These studies assess real-world data but can only indicate correlation and cannot definitively establish causation.
So what are the results of the above when it comes to the COVID-19 vaccines:
1. COVID-19 Vaccine Results from Manufacturer RCTs
Efficacy
Wilf entirely overlooks the fact that the original RCTs achieved the “95%” efficacy label through the use of several methodological maneuvers. These trials had significant issues, including:
Non-representative study population
Testing discouraged <7 days after vaccination
Lack of relevant clinical endpoints
Early unblinding
High dropout rates
Possible unblinding via PCR tag
Unknown mechanism of immunity
Neutralizing antibody timeline mismatch
A detailed article including sources can be found here.
Wilf correctly points out that the studies show no sign. death signal. However, it is important to note that the study population was exceptionally healthy, as individuals at high risk for severe COVID-19 were explicitly excluded. This raises a significant concern: How can a study, primarily designed to evaluate protection against severe illness and death, demonstrate any meaningful effect when the very people most likely to benefit were excluded from participation?
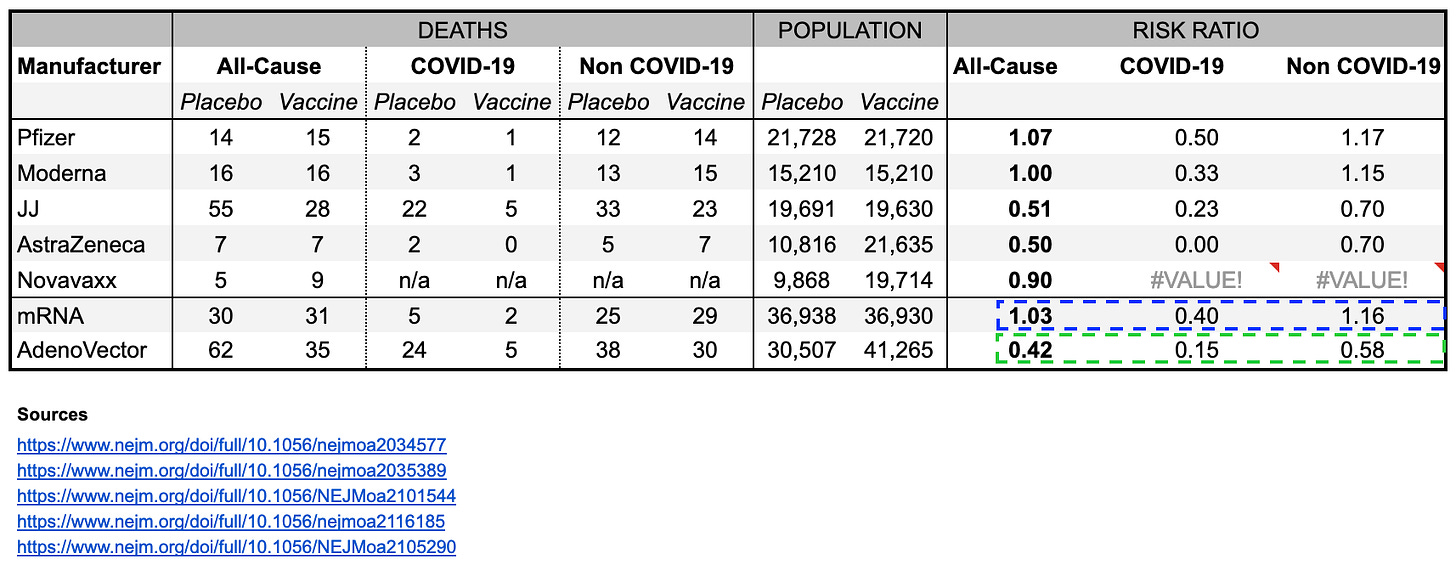
The endpoints used in the studies were inadequate for establishing clinically meaningful efficacy. The only truly relevant endpoint was all-cause morbidity and mortality, yet only mortality was reported, leaving a significant gap in assessing the vaccine’s overall impact. Here’s an overview of the prospective, double-blind, placebo-controlled trials that were conducted for vaccines later administered in the West:
mRNA Vaccines:
All-Cause Mortality: No benefit (RR = 1.03)
COVID-19 Mortality: Reduced (RR = 0.4)
Non-COVID Mortality: Elevated (RR = 1.16)
Adenovector Vaccines:
All-Cause Mortality: Significant benefit (RR = 0.38).
COVID-19 Mortality: Strong reduction (RR = 0.18).
Non-COVID Mortality: Unexpected reduction (RR = 0.5), raising concerns of imbalance or trial irregularities.
Evident from the above data, the mRNA vaccines, the most commonly used in the West, show no benefit for all-cause mortality (RR = 1.03) and may increase non-COVID deaths (RR = 1.16). Adenovector vaccines report suspiciously large reductions in non-COVID mortality, raising concerns about potential trial issues. This has been confirmed by a peer reviewed article by Benn et al., 2023.
Notably, all trials were unblinded early, with observation periods lasting less than 3 months (e.g., Pfizer). This limited timeframe is inadequate for detecting medium- to long-term side effects, making it impossible to fully assess potential harms. While follow-up periods were longer, the early unblinding disrupted the balance between groups, rendering proper comparison of all-cause mortality unreliable.
Conclusion: None of the RCTs convincingly demonstrated lives saved, leaving the potential for harm unresolved due to the much healthier population and short observation.
2. Confirmed reports and harm
There are numerous documented reports and signals that highlight potential harms. Here is a brief overview of the evidence. Any such documentation is sufficient to establish that harm is possible:
Individual Case Reports
Examples such as Roy Butler, Natalie Boyce, who both passed away several weeks after vaccination, underscore potential risks. Numerous similar reports have been documented and are identifiable in public records.
Myocarditis Autopsy Study
Among 25 individuals who died unexpectedly within 20 days of vaccination, autopsies identified myocarditis as the likely cause of death in five cases. Additional studies have examined other adverse effects, such as thrombosis and other potentially fatal side effects.
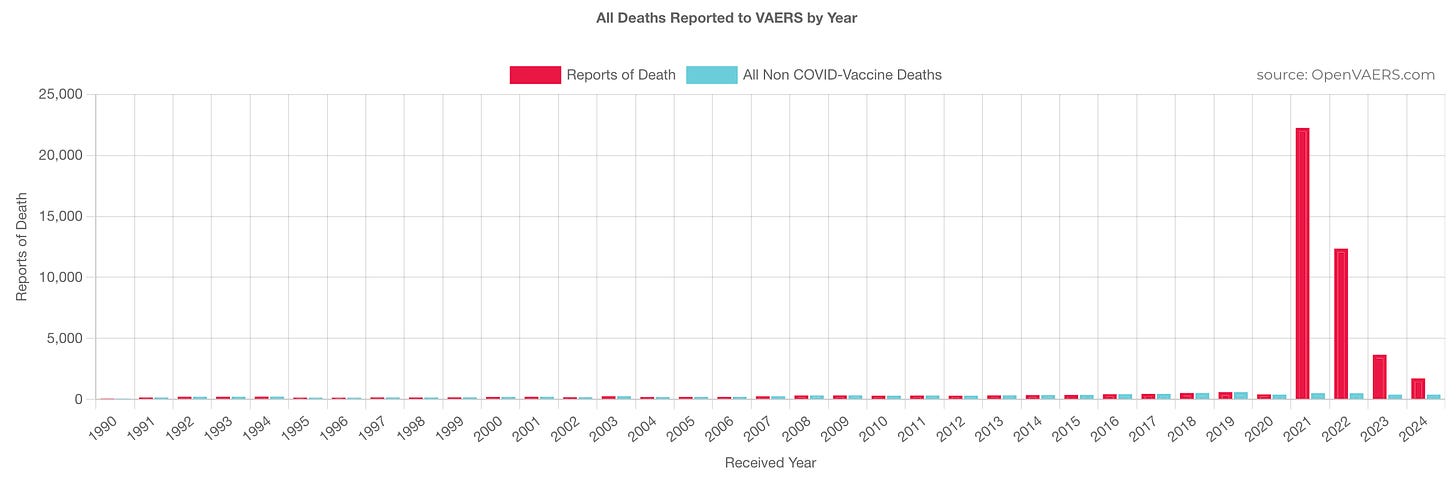
VAERS Data
The U.S. Vaccine Adverse Event Reporting System (VAERS) recorded a significant signal of adverse events following vaccine rollout. While these reports do not establish causation, the sheer magnitude of the signal provides a strong indication of potential risks that warrant further investigation.
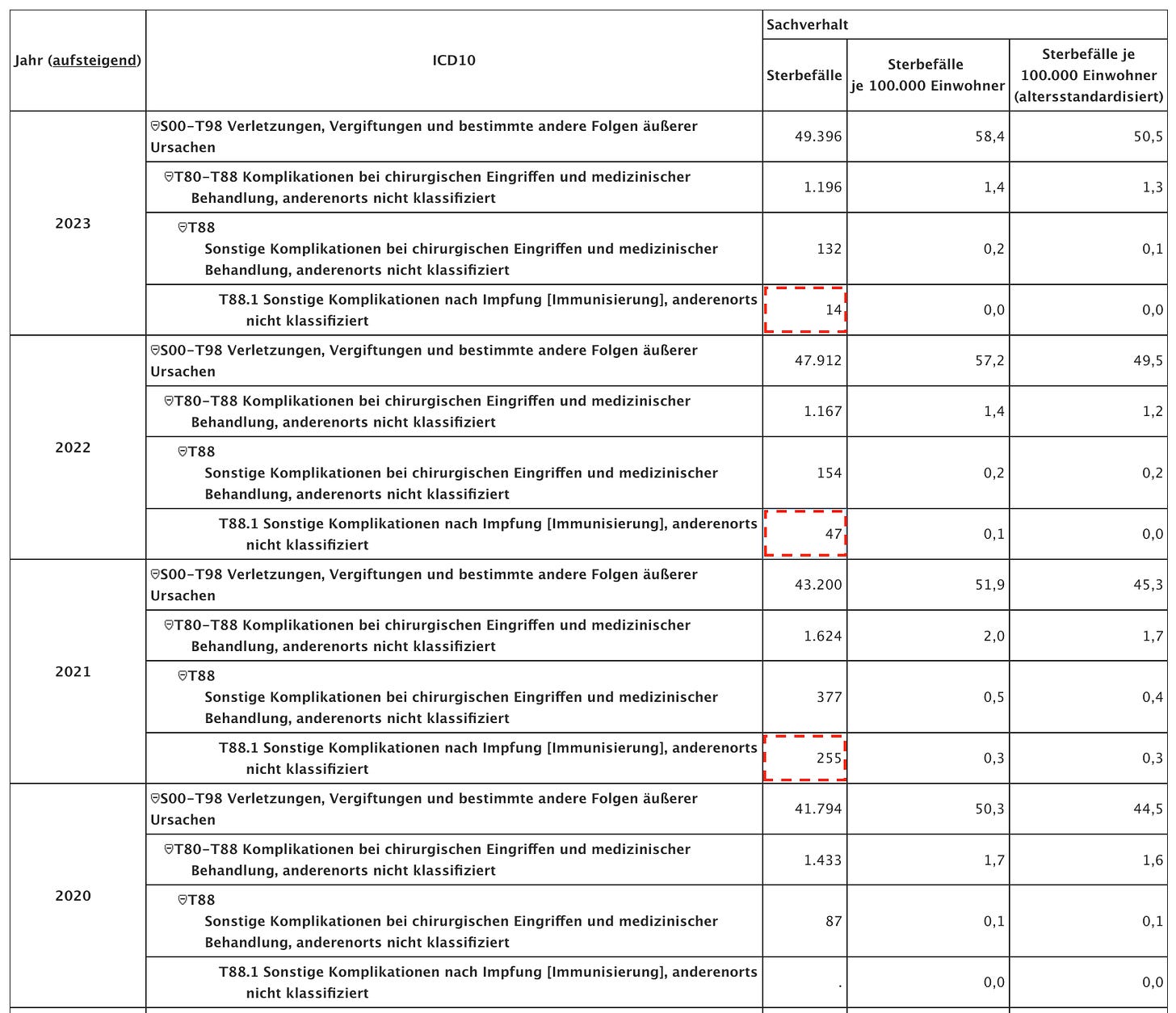
Official German Cause of Death Statistics
The German Statistical Office in Germany has recorded 316 deaths under the underlying cause of death category for T88.1 “Other complications following immunization, not elsewhere classified” in 2021. This number was 255 in 2022, 47 in 2023, and a total of 316 over the past four years. Notably, there were no deaths recorded in this category in the previous several years.
The Statistics Office has confirmed that at least a significant portion of these cases can be directly attributed to COVID-19 vaccination. A more detailed FOIA request by me is currently pending.
Interim Conclusion
As you can see, section 1, the original randomized controlled trials, did not demonstrate any overall mortality benefit; section 2, harms, clearly shows evidence of several hundred deaths in Germany alone (1 in ~200k vaccinated); a rough global estimate (based on the confirmed German mortality incidence) brings the number of deaths to over 27,500 (5.65b vaccinated).
3. Observational Studies
This brings us to the third aspect: the observational studies, which Wilf frequently cites. These studies must clearly and unequivocally demonstrate a substantial positive effect to offset the observed net harm. However, from a technical standpoint, the debate should already be resolved, as observational studies cannot establish causality. Despite this limitation, let us take a closer look and dissect them further:
Analysis of the entire Hungarian population
Wilf mentions a study from Hungary, examining all-cause mortality over a brief 4-month period, only two of which experienced excess mortality. It is is so fundamentally flawed that the authors withheld both the underlying data and their calculations, and stopped responding to several inquiries:
Exclusion of partially vaccinated adults: UK data shows highest mortality in this group.
Health-related variability: Structural indicators vary across vaccination groups, confounded by general health status.
Moderna lower survival probability: Highlighted in Figure 2.
Short observation period: Only 4 months (Apr-Aug 2021), highest mortality observed in partially vaccinated.
Person-year miscalculation: Potential errors if vaccination date reporting is inaccurate.
Conclusion: The study fails to provide valid evidence of vaccine efficacy due to its very short observation period (4 months), significant confounding, and incomplete cohort comparisons (e.g., ever vaccinated vs. unvaccinated). Similar to the recently published Norwegian study, it cannot demonstrate that mortality rates are indeed equal to or lower in the vaccinated cohort compared to those without the intervention.
Comparing ACM across countries and time
Wilf asserts that vaccination and COVID-19 incidence are the key determinants of excess deaths. However, vaccination has not demonstrated any positive impact on the presumed spread or incidence of the virus to begin with, as randomized controlled trials (RCTs) have not shown that vaccines have saved any lives. Moreover, COVID-19 data is neither reliable nor comparable, as it was not collected in a controlled manner from a statistically representative population sample.
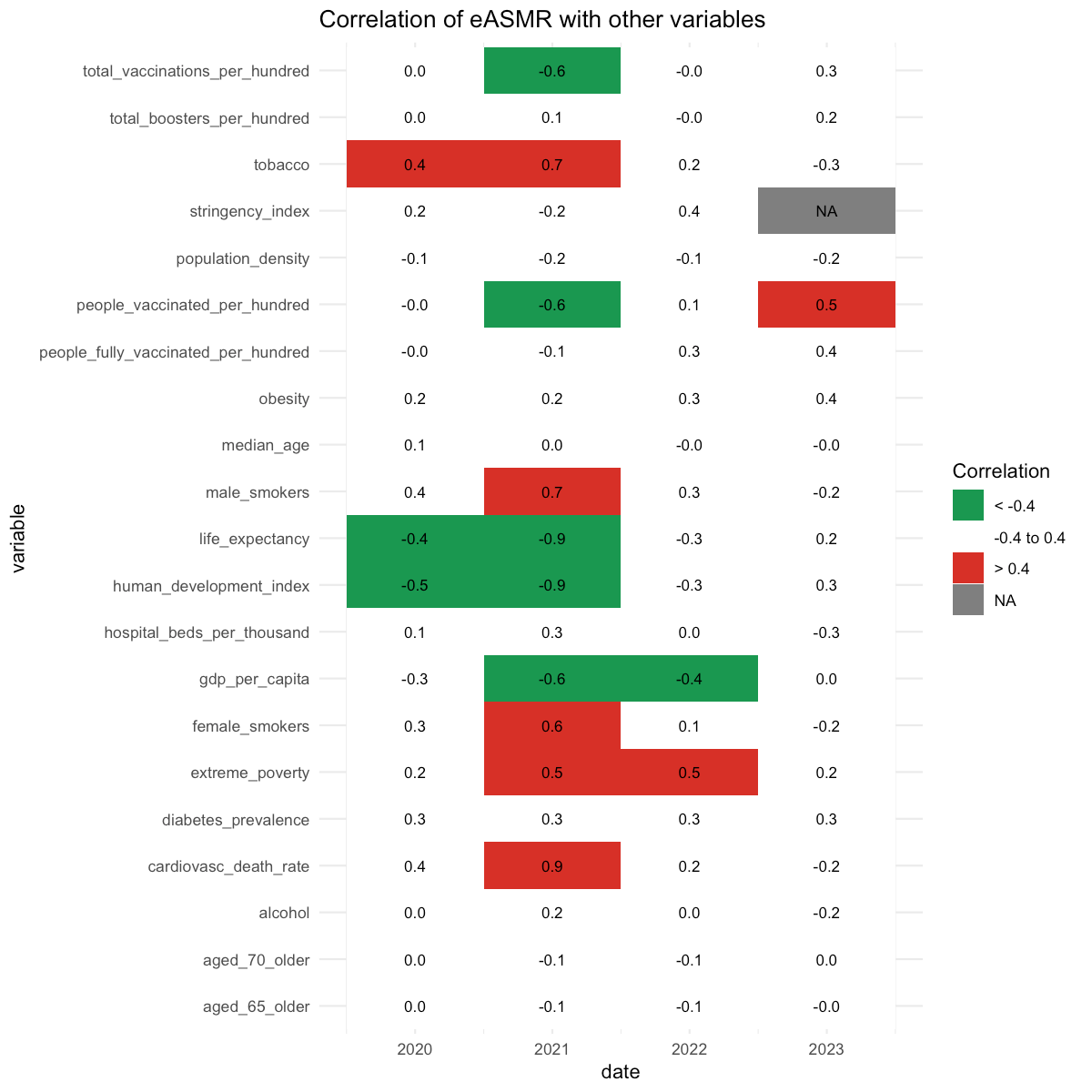
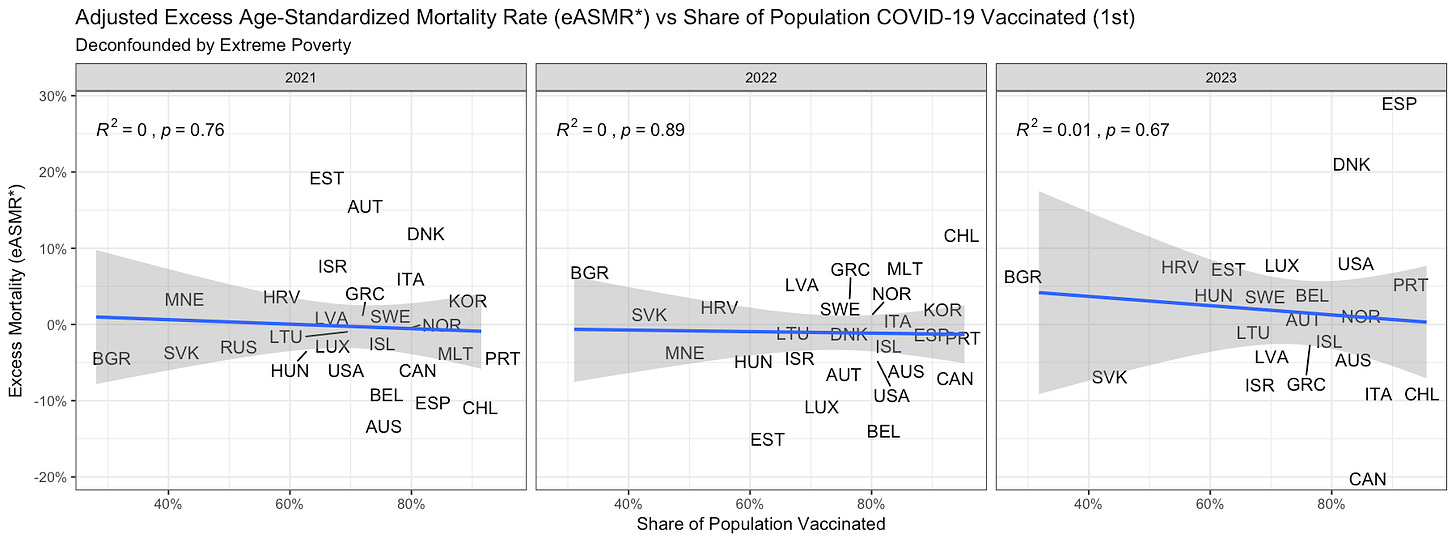
When comparing all-cause mortality across countries, it becomes evident that while vaccines appeared to have an impact in 2021, several other confounders are the primary drivers of excess deaths.
For instance, after adjusting mortality rates for the confounding variable “extreme poverty,” any positive correlation with vaccination disappears entirely.
The significant impact of poverty on mortality has been well-documented, as highlighted by Ioannidis et al. (2023): “Excess deaths (as a proportion of expected deaths, p%) were inversely correlated with per capita GDP (r = -0.60) and positively correlated with the proportion living in poverty (r = 0.66).”
ED of Republicans and Democrats
The study’s findings may highlight real disparities in excess mortality, but its several major methodological issues severely limit the validity of its conclusions. The relevance of political affiliation is likely overstated or arbitrary. Instead, the differences likely stem from:
Movement During the Pandemic: Population movement, especially starting in mid 2020, after the initial lockdowns, may have severely affected the AI-based name-matching algorithm used to link voter registration and mortality records. This could lead to significant errors in matching mortality to the individuals.
Limited Timeframe: The analysis only extends until 2021. To robustly attribute the observed effects to vaccination, data beyond 2022 is essential. If mortality rates converge after 2021 back to no differences between R/D voters, it would indicate vaccination effectiveness; if not, it could suggest confounding factors or other effects.
Societal and Long-Term Factors: Stress, lockdown-related effects, economic hardship, drug overdoses, and other long-term societal impacts cannot be ruled out as contributors to excess mortality, disproportionally affecting R voters.
State-Level Discrepancies: The presumed effect is much less visible in Florida but more pronounced in Ohio, suggesting the observed differences may result from factors other than vaccination or party affiliation.
Age Adjustment Issues: The study only adjusts for broad age bins. Republican voters, being older on average, may exhibit higher relative effects of mortality impact, which could bias the results.
Short Baseline Fit: The baseline is based on a two-year fit (2018–2019) using a Poisson regression model at the county-by-party-by-age level. This short period risks producing artifacts, especially given seasonal or structural trends in mortality. Additionally, no confidence intervals (CIs) are provided for these baseline estimates. This fact alone should immediately dismiss the validity of the study.
No Adjustment for Sex or Race: The study does not account for sex or race, both of which are critical factors in mortality and could confound the observed results.
Timing of Divergence: The divergence in mortality begins much earlier than the smoothed line suggests, around mid-2020. This timing predates vaccine availability, suggesting that non-vaccine factors played a significant role.
Data and Code Not Publicly Available: The lack of public access to the dataset and analysis code prevents independent verification and replication of the study’s findings, reducing transparency and credibility.
The study’s findings are significantly undermined by its methodological flaws. The observed differences in excess mortality, attributed to political affiliation, are likely a proxy for other structural and behavioral factors, such as rural vs. urban residence, socioeconomic disparities, healthcare access, and vaccination behavior. A more robust analysis would require individual vaccination data, adjustments for key demographics, and a longer timeframe to draw valid conclusions. The focus on political affiliation appears overstated and overly politicized.
EDs are Covid
Wilf claims that all excess deaths in the US are caused by COVID-19 but overlooks critical nuances. Several regions have shown no significant excess mortality, even as the US recorded double-digit excess rates, bringing into question the underlying health emergency to begin with. Additionally, Wilf misunderstands how ICD-10 codes for COVID-19 are determined. There is a straightforward explanation for why COVID-19 deaths often align with excess deaths — but this phenomenon is primarily observed in western and wealthy countries.
COVID-19 Death Classification in Western Countries
Most western countries have incentivized the classification of seasonal respiratory illnesses as COVID-19. Additionally, many apply their own death certificate modeling systems, such as the CDC’s NVSS/MMDS. Source
Origin & Clinical Relevance of Found Sequence
The origin & clinical significance of the identified sequence remains unknown to this day. Source
PCR Primer Similarity to the Human Genome
The PCR primers used for COVID-19 testing have a high similarity to the human genome. Source
Limitations of Wastewater Surveillance
Even wastewater surveillance cannot substantiate claims that COVID-19 was a novel virus or provide precise assessments of viral levels. The method involves pooling genetic material from multiple strains and individuals, complicating attribution. Furthermore, no pre-2020 data exists to validate these techniques as a reliable control. Source
Clinical Validation of COVID-19 PCR Tests
The COVID-19 PCR test has never undergone clinical validation to demonstrate specificity or predictive accuracy for diagnosing COVID-19. In hospitals, many positive results were incidental, meaning individuals tested positive but were not ill with respiratory conditions like COVID-19. Source
All of this raises significant doubts about whether the excess deaths can genuinely be attributed to an assumed novel pathogen.
ED in countries with Zero Covid
Wilf asserts that several countries were able to “stop COVID-19 for a long time,” but this claim does not hold up to scrutiny. No mitigation measures have been scientifically proven to significantly halt the spread of COVID-19 or any respiratory disease.
The countries cited are predominantly island nations, which may have created the appearance of controlling the virus through border closures and quarantine measures. However, scientific evidence does not conclusively support the effectiveness of these strategies in completely stopping viral spread. Instead, the observed outcomes may have simply sustained an illusion of control within the population.
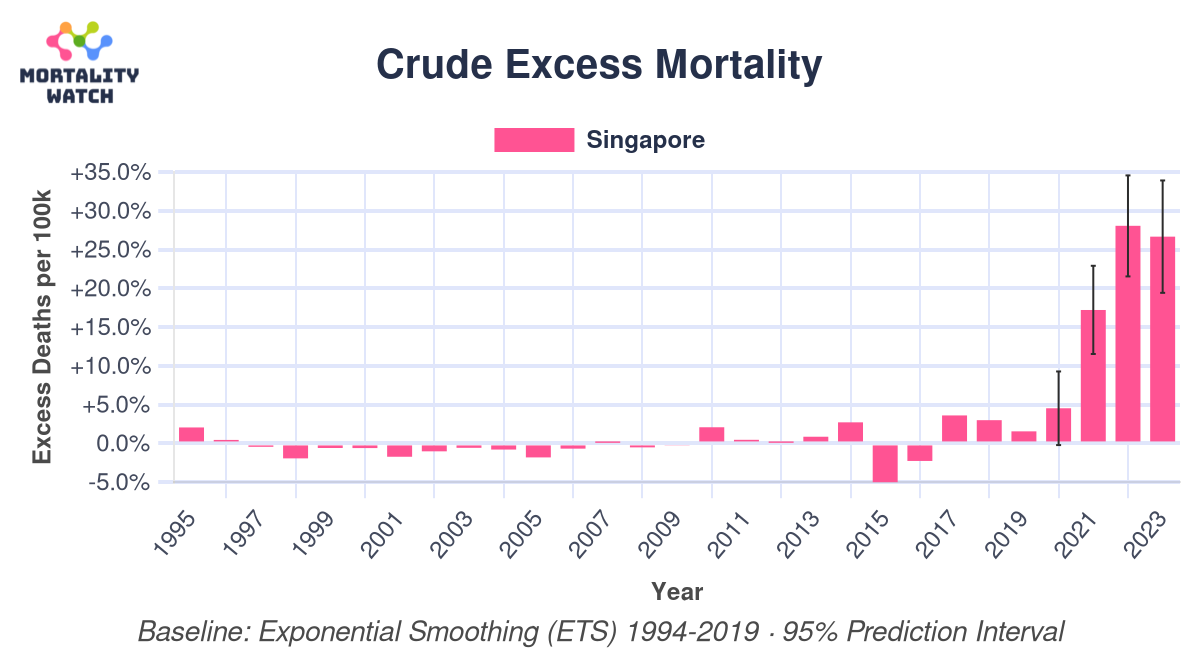
Notably, after reopening, many of these highly vaccinated countries experienced significant excess mortality over multiple years. For example, Singapore, with a vaccination rate of 94%, recorded substantial excess mortality, especially in the elderly population—but only starting in 2021.
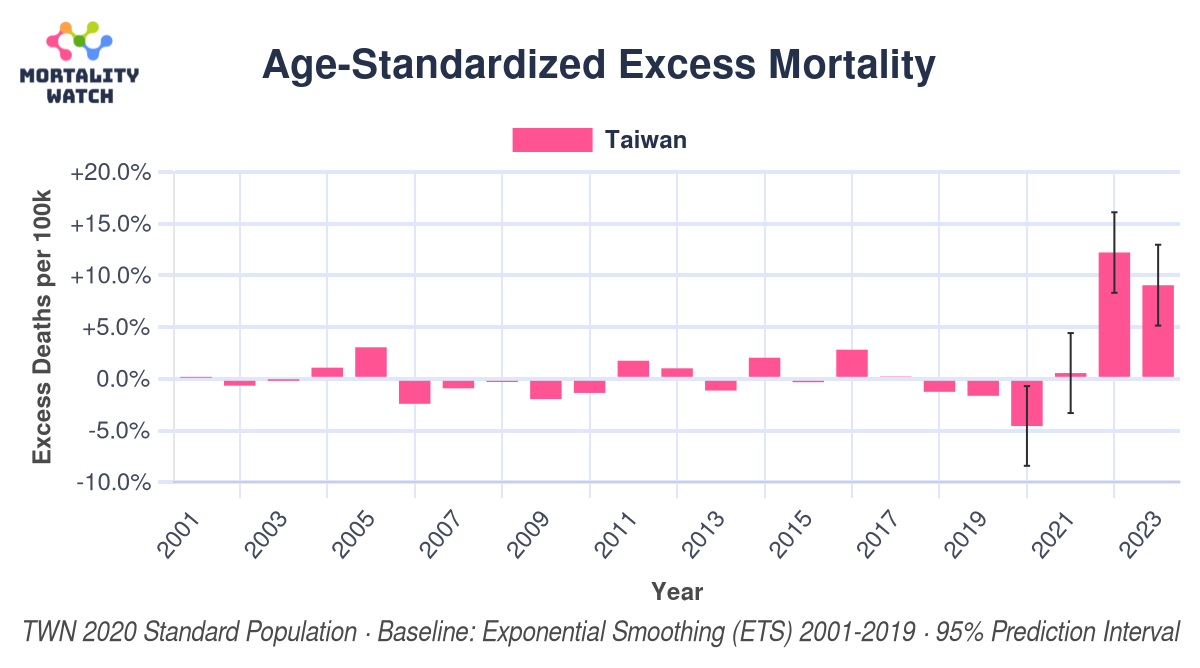
Similarly, Taiwan, another highly vaccinated nation, experienced a comparable trend.
These figures challenge the assumption of a highly effective vaccine. In contrast, some countries with lower vaccination rates—such as Luxembourg, Denmark, and Germany—reported little to no notable excess mortality. A full ranking can be found here.
Wilf should investigate whether these deaths could be linked to mechanisms such as Antibody-Dependent Enhancement (ADE) or other vaccine-related factors that may exacerbate disease outcomes. Alternatively, he should assess whether these excess deaths are genuinely attributable to SARS-CoV-2 or if other contributing factors better explain the observed trends. Data from the Mortality Watch Excess Ranking, based on age-standardized deaths and a conservative 3-year pre-pandemic baseline, reveals at least two dozen countries that did not exhibit statistically significant excess mortality during the 2020–2023 period. These findings challenge the notion of a universally impactful pandemic and warrant further scrutiny into regional disparities and underlying causes.
Saved by the Vaccine
In-Vitro Studies
Wilf’s argument regarding “neutralizing antibodies,” which are demonstrated in vitro to neutralize the virus, is fundamentally flawed. Antibodies are not inherently specific to this virus, and their levels are merely determined by concentration (titers). In fact, most antibodies may be found in small quantities across all individuals, rendering their purported specificity questionable.
Moreover, no studies have conclusively shown a correlation between antibody levels and improved clinical outcomes. As such, the argument lacks empirical support and is ultimately moot.
Israeli data
The presented data is insufficient to establish any meaningful conclusions about vaccine efficacy, primarily due to the use of non-comparable cohorts and the presence of confounding factors. Even in the provided charts, there is no clear effect over time; instead, the lines remain consistently different. This pattern strongly suggests that the data is confounded, making it unreliable for drawing causal inferences about vaccine impact.
Effect on cases and CFR
Any calculation involving COVID-19 data is inherently flawed, as it does not originate from a statistically representative population sample. Furthermore, the data is highly confounded by factors such as the number of tests conducted, testing policies, and variations in health status among populations. As a result, these calculations cannot be considered reliable evidence for determining efficacy.
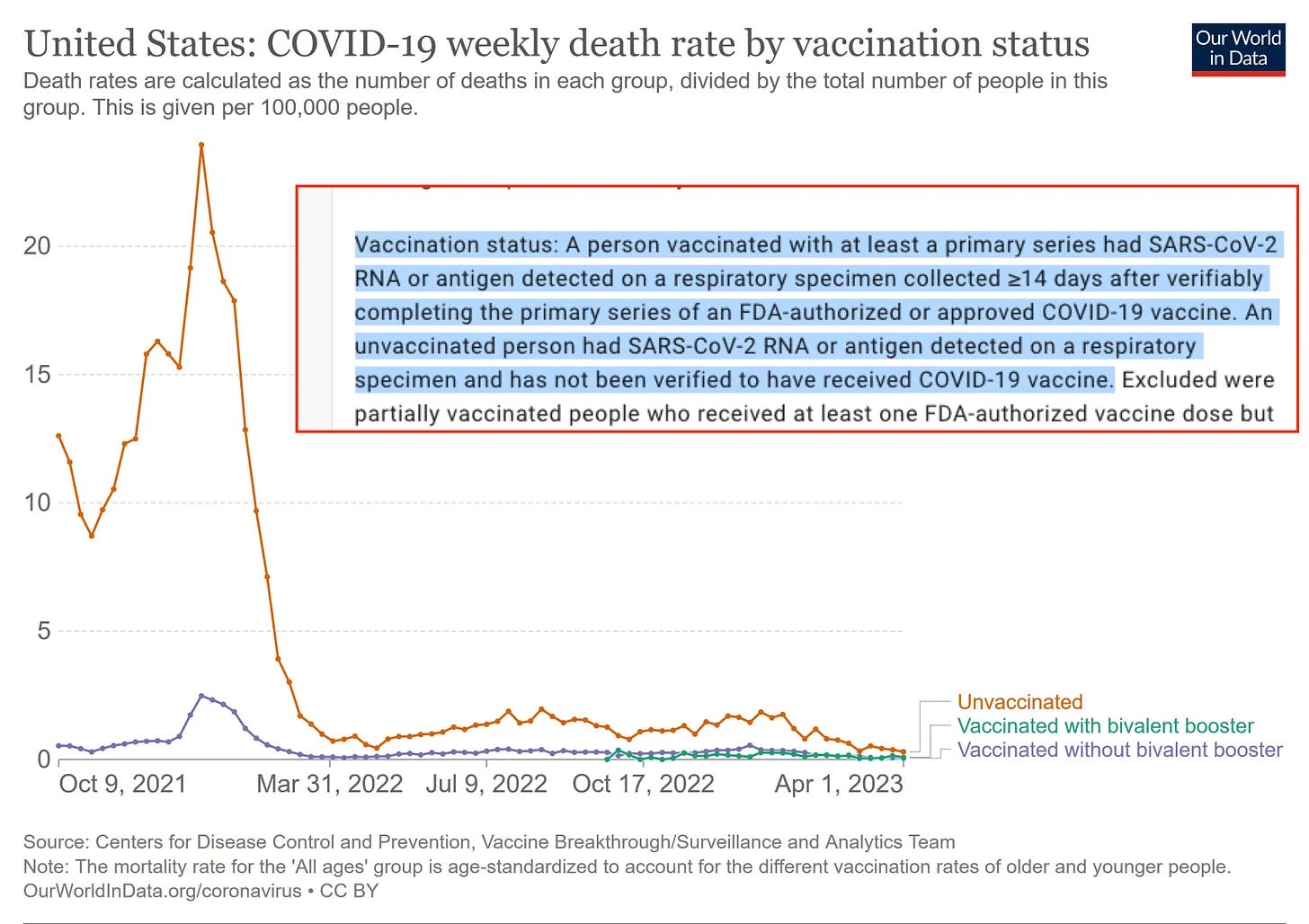
Covid Deaths by Vaccination Status
Wilf prominently references U.S. data on COVID-19 deaths by vaccination status, as presented on OWID. However, this data is fundamentally flawed, as it is not publicly available in its entirety. The data presented only includes mortality rates, without providing the actual death or population figures used for calculations, making it impossible to verify or properly analyze.
In summary, the chart suffers from at least three major issues:
Use of unreliable data
The analysis relies on biased, uncontrolled, and unvalidated COVID-19 testing data, rather than objective, gold-standard metrics like all-cause mortality.
Exclusion of relevant data
Vaccinated individuals are only considered “fully vaccinated” 14 days after their second dose. This approach omits at least five critical weeks of data, including the period immediately following vaccination, which could influence outcomes.
Misclassification of vaccination status
The “unvaccinated” group likely includes a significant number of vaccinated individuals whose vaccination status could not be matched or verified. For example, in Germany, approximately 80% of individuals’ vaccination statuses are unknown, leading to severe misclassification.
These issues are not unique to U.S. data; similar problems exist in datasets from other countries. On the other hand, data from New Zealand provides a contrasting perspective. It shows that mortality rates for vaccinated and unvaccinated groups are similar, and the country experienced no statistically significant excess mortality during the pandemic. This, along with Sweden’s experience, serves as evidence that there was no widespread health crisis requiring extraordinary measures to begin with.
Covid Deaths by Vaccination Rates
The same fundamental issues outlined above apply here: COVID-19 data is inherently unreliable, and all-cause mortality metrics are heavily confounded. After accounting for these confounding factors through proper deconfounding methods, it is evident that no significant vaccination effect remains.
Calculating Lives Saved
Thus, the entire calculation for “lives saved” can be outright dismissed, as it relies on flawed models. These models, for example, assume a constant Case Fatality Rate (CFR) without considering whether the CFR is accurately measured in the first place. This methodology suffers from the same issues I outlined in my article “Did the vaccine save 20 million lives?”
Summary
Randomized Controlled Trials (RCTs) provided no evidence of efficacy for the general healthy population—no lives saved and no data reported on clinically relevant morbidity. Furthermore, these trials were not designed to adequately assess safety for older, frail individuals or those at higher risk, on top of having several methodological issues that may even have been designed intentionally to achieve the intended outcome (“the illusion of efficacy, through not clinically relevant data”).
Hard evidence, including ICD-10 coded vaccine-related deaths, confirmed autopsies, and detailed case reports, clearly demonstrates that these vaccines can cause harm and even death.
Observational studies, despite their volume, are riddled with methodological flaws that render their conclusions unreliable. Issues such as insufficient evidence, methodological weaknesses, and pervasive confounding are pervasive. Additionally, societal and lockdown measures disproportionately impacted unvaccinated individuals, especially from mid-2021, when significant societal pressure and mental stress were placed on them. Social exclusion and related stress led to further disruptions, including relocation (skewing population data/denominators), changes in life routines (e.g., commuting, eating habits), and increased drug use, complicating the interpretation of these studies even further.
These considerations underscore that there is no solid basis to claim that the net effect of vaccines can ever be shown to be causally positive. The belief that “vaccines work” appears to remain a matter of faith rather than scientific evidence. 😉




Excellent work, thanks. I came to a similar conclusion.
https://doi.org/10.13140/RG.2.2.12370.57281/1
Well-written and of course, I concur!